IMPROVE MY GAME
Articles
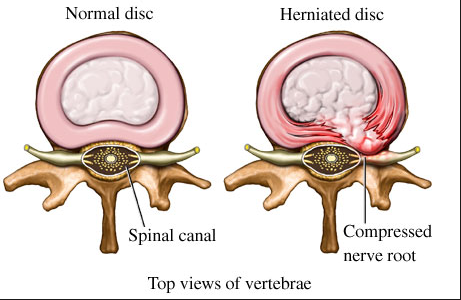
When Surgery is the Right Treatment for Your Herniated Disc

Image from Spine-health
What is a herniated lumbar disc and how does it occur? More importantly, how does a herniated disc affect my golf swing and how can I regain my swing once I have recovered from my injury? Herniated lumbar discs are a very common problem affecting 1.6% of the US population at any one time. It is most common in people between the ages of 30 to 55 and affects men twice as often as women.
The question of whether surgery is an effective treatment for herniated lumbar discs has been extensively studied and reported in a landmark study entitled the Spine Patient Outcomes Research Trial (SPORT). Essentially, what the study found was that most patients recovered from herniated discs without surgery from a combination of conservative therapies such as physical therapy, spinal manipulation, spinal injections and anti-inflammatories. However, when symptoms persist or if a patient had neurologic problems, then surgery is a safe and effective treatment.
At what point is surgical intervention required for a lumbar disc pathology? Conservative treatments providing limited results. #commonquery
— LanceGillPerformance (@LGP_Inc) January 6, 2017
It is obvious that when you have pain from a herniated disc, you are not going to be in any condition to swing a club. As soon as the sciatica pain begins, there is some weakness and loss of muscle control in the distribution of the nerve. This muscle weakness may be dramatic, such as a floppy foot, or it may be imperceptible. However, even when your pain resolves your swing can be temporarily or permanently altered because of this weakness. Therefore, even after you recover from your sciatica you are at risk of re-injuring yourself because the muscles that stabilize your hips and allow rotation are weak and will cause swing faults such as early extension and reverse spine angle. Not unexpectedly, these are the most common swing faults that result in back pain. Let me explain how this happens.
The most common levels for discs to herniate are at the L4-5 and the L5-S1 levels. The nerves that are affected are the L4, L5 and S1 nerve roots. If you have spent any time on mytpi.com you will know that the “King” of the golf swing are the “Glutes”.
The gluteus medius and gluteus minimus are supplied by the L4 and L5 nerves. The gluteus maximus is supplied by the L5 and S1 nerves. So if any of these nerves are affected, the stability of the hips is altered (bridge with leg extension test). Furthermore, the associated sensory disturbances that can result from a pinched nerve can cause proprioceptive dysfunction resulting balance issues (single leg balance test). These will produce the predictable swing faults.
So the most common nerves to be affected by lumbar disc disease are the muscles that innervate the “King” of the golf the swing. It is no surprise then that even a single episode of sciatica can lead to an inefficient golf swing that predisposes you to repeated episodes of pain. I often explain to my patients who are considering a discectomy that surgery sets the stage for recovery. It is of paramount importance to undergo a systematic postoperative rehabilitation program. This should be followed by a graduated training program to regain muscle control. This will increase the likelihood that you will regain your previous level of function and minimize further injury.
If pain from a herniated disc persists despite conservative treatment or if there is muscle weakness present in the distribution of the nerve then surgery is a safe and effective treatment option. I prefer minimally invasive surgical techniques to traditional methods as they are less destructive to the normal spinal anatomy.
The traditional surgical procedure to treat herniated discs is called a laminectomy/discectomy. This procedure involves stripping the muscles off of the spine and opening a window into the spinal canal. This is accomplished by removing a portion of the roof of the spine called the lamina – hence the term laminectomy. It also involves shaving down part of the facet joint. The facet joint is one of the structures that provides mobility and stability to the spine. Removal of these structures allows access to the spinal canal and visualization of the nerves and disc herniation.
While this is an effective surgery to remove the herniation that causes injury to the paraspinal muscles (more specifically, the multifidus muscles) by devascularizing and dennervating them, there are significant drawbacks. The multifidus muscle is an important muscle of the spine as it helps to provide segmental stability. When the muscle does not get blood or nerve input it becomes weak and atrophied. It is well known that injury to or weakness to the multifidus muscle is a major contributing factor in developing chronic back pain. Furthermore, this is one of the muscles that physical therapist focus on strengthening when you are in rehab trying to avoid surgery. So the treatment to avoid surgery and the surgery itself are counteractive and predispose patients to chronic low back pain.
Lumbar discectomy has evolved and newer, minimally invasive techniques have become more common. Muscle sparing techniques have been developed in an effort to reduce injury to the multifidus muscles. This technique employs a series of progressively larger dilators to create a channel to the spine so a small window in the roof of the spine can be created. A small amount of the joint is removed. The operating microscope is then used to illuminate and magnify the area where the nerve and herniation are located. The herniation can be removed while minimizing injury to the multifidus.
In fact, in the video you can see that as the retractor tube is removed, the muscle appears normal and healthy. In my practice, this surgery is an outpatient procedure performed under general anesthesia through an 18 mm incision. I inject the operative area with a long acting local anesthetic to minimize the amount of narcotic pain medication that is required after surgery. The advantage of this MIS procedure is that patients tend to have a faster recovery with less pain than a traditional open discectomy.
My preferred method of discectomy is even less invasive. I want to avoid any injury to the multifidus muscle or facet joint altogether, so I exploit the natural window into the spine called the neuroforamen. The technique involves placing a needle through the flank muscles down through the hole where the nerve exits the spine. A series of dilators followed by reamers are used to remove a small amount of bone to enlarge the size of the foramen and introduce a cannula. This has no adverse impact on the stability of the spine. An endoscope is then inserted and the nerves are visualized and the disc herniation is then removed in a similar manner to the other procedures. Technically speaking, the procedure is called a transforaminal endoscopic discectomy but I call it the Joimax procedure after the German company that perfected it. In my practice, this procedure is performed with the patient lying on their side and lightly sedated. This allows me to interact with the patient while performing the operation. This is also an outpatient procedure and patients experience less side effects with sedation than with general anesthesia. Since we do not injure the back muscles, this is my preferred method for golfers.
While I consider surgical treatment of lumbar disc herniation to be a last resort, it is an effective treatment option for people whose pain and dysfunction will not go away. The advent of new minimally invasive techniques minimizes the likelihood that back surgery will end your golfing career.
Click Here to read the SPORT Trial
Click Here for recent study comparing Joimax procedure to MIS discectomy
Click Here to learn more about the Joimax procedure

Dr. Paul Houle is a neurosurgeon specializing in minimally invasive spinal procedures. He received his medical degree from Boston University School of Medicine in Boston, and completed his residency in neurosurgery at the University of Georgia. He is the Chief of Neurosurgery at Cape Cod Healthcare (find them on Facebook). Dr. Houle attended TPI Level 1 in 2016 and is TPI Certified.